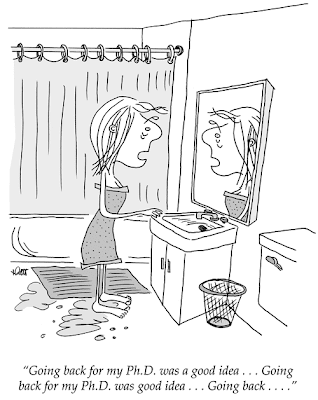
Yes, I'm back. So the semester is just plugging along and I'm now over the half-way point in the semester. At some moments it has seemed agonizingly slow, and other moments I can't believe how fast it's going. I hope the latter remains true for the entire program!
So what have I learned? What pearls of wisdom can I share with you? Hum...well, truthfully I don't think you'll find them any bit interesting. So instead of content, we'll talk big picture. I do think I am starting to get the hang of the PhD-way-of-thinking. It's a slow process, granted, but I think it is starting to come together.
It's funny though, because professors will ask, "How does this tie into your own area of interest for research?" But most of the time I think they keep you so busy there's barely any time to consider how this abstract thought relates to trauma. It's actually all the quantitative work that I like the best. All this foo-foo abstract philosophy business just doesn't move me.
But the good news is I hear the first year is the worst. Actually, I've even heard it starts to get better by second semester. It sounds like the general process is you start the program with the most abstract content and then it continues to narrow down to more concrete information as you move along. Boy , I can not wait for concrete! I think acute care people in general don't live, nor want to, in some nebulous world. So, I will continue to keep you posted. Here's hoping the fog clears soon!
Monday, November 1, 2010
Friday, October 1, 2010
Pardon the time lapse again
Well, when I posted that the PhD was likely going to involve a new way of thinking, I don't even think I realized to what extent that might be. Indeed, it is different. On one hand, it is very hard to go from being a very proficient clinician to... studying theory and philosophy.
Sadly, on the other hand, I don't even think that I can say it's hard. More or less, I feel intellectually bored. Sure, they give oodles to read, and now oodles of writing is coming down the pike, but I can't really say that I feel mentally stimulated.
Instead I find myself doing other things, like this. :) I even signed up for a 7- week course through the local community. I'm getting a chance to run more than I ever could while working as a Trauma NP. My other projects are getting valuable attention.
Yet my classmates, albeit there's only 4 of us total, say how overwhelmed they feel. I sort of feel like, "Am I missing something?" Okay granted, there's plenty to do, but it honestly feels more like busy-work than bearing true value to the real world. I'm looking for meat & potatoes. Substance. Not philosophy.
Now I don't want to be too much a downer, because that's not me, so I'm just going to hold my breath and hope for the best. Let me find a silver lining- perhaps learning how I can affect large-scale change will be next semester.
Sadly, on the other hand, I don't even think that I can say it's hard. More or less, I feel intellectually bored. Sure, they give oodles to read, and now oodles of writing is coming down the pike, but I can't really say that I feel mentally stimulated.
Instead I find myself doing other things, like this. :) I even signed up for a 7- week course through the local community. I'm getting a chance to run more than I ever could while working as a Trauma NP. My other projects are getting valuable attention.
Yet my classmates, albeit there's only 4 of us total, say how overwhelmed they feel. I sort of feel like, "Am I missing something?" Okay granted, there's plenty to do, but it honestly feels more like busy-work than bearing true value to the real world. I'm looking for meat & potatoes. Substance. Not philosophy.
Now I don't want to be too much a downer, because that's not me, so I'm just going to hold my breath and hope for the best. Let me find a silver lining- perhaps learning how I can affect large-scale change will be next semester.
Thursday, August 26, 2010
A new way of thinking
Well, Orientation has begun...and the nerves are mounting. I haven't even had my official PhD intro day yet, where I'm sure I'll hear all the nitty-gritty and panic even more. But even having lunch with a 4th-year PhD student was enlightening. I am starting to realize I will have to embrace a new way of thinking. I suppose there was some mental adjustment, if I remember, when I was learning how to practice as a nurse practitioner from bedside nursing. But this change in thinking seems even more dramatic to me. To this point, all of my training and experience in nursing is in a clinical context. But now I feel I am leaving the clinician in me behind, and have to cultivate the researcher in me. As excited as I am about learning how to be a researcher, prolific publisher, and professional expert on my topic, I realize the task is daunting. Nonetheless, I hate to completely give up clinical practice 100%; it feels weird. I asked the 4th-year PhD student her opinion on working clinically at least one day a week. She did not recommend it due to the rigors of the program. She said I will be so busy and overwhelmed that I should avoid it, if possible. While I realize she is probably right, it is a bit sad. Yet, since I can see I am in for a big change, I will certainly heed any cautionary tales at this point.
Tuesday, July 27, 2010
Oops- hiatus
Oh my goodness, look how much time I let lapse! I sure didn't mean to. But I must say, a lot has happened since I last posted. Sadly, I no longer work as a trauma NP. Not that that comes as a surprise but still sad to move on. As much as I loved my job, I had to give it up to start the new chapter of my life as a PhD student. I have now relocated across the country. And let me say, that was no easy feat.
Actually, I moved a little early because I was going to study Public Health in Boston over the summer. Well, things didn't turn out as planned. Long story short, I ended up with a moving company scam that caused me to miss orientation and the start of [summer] school. I could NOT get my furniture, and I spent so much time absorbed by the scandal. Fortunately, I did get my stuff, eventually .
So now that I have finally sorted out the all the disasters from the move, I've had a chance to start looking at what's to come. Of course, I've ended up with more time now than I had expected, since my summer studies got cut out of the mix. So, with time to stop and breathe for the first time in a long time, I think I am now starting to realize I am really going back to school. It started to become real when I saw the orientation schedule and the courses I'll begin this fall. I am getting excited, although I have to admit, a bit nervous too. But I am not one to do well with much down time, so I am anxious to get started.
Actually, I moved a little early because I was going to study Public Health in Boston over the summer. Well, things didn't turn out as planned. Long story short, I ended up with a moving company scam that caused me to miss orientation and the start of [summer] school. I could NOT get my furniture, and I spent so much time absorbed by the scandal. Fortunately, I did get my stuff, eventually .
So now that I have finally sorted out the all the disasters from the move, I've had a chance to start looking at what's to come. Of course, I've ended up with more time now than I had expected, since my summer studies got cut out of the mix. So, with time to stop and breathe for the first time in a long time, I think I am now starting to realize I am really going back to school. It started to become real when I saw the orientation schedule and the courses I'll begin this fall. I am getting excited, although I have to admit, a bit nervous too. But I am not one to do well with much down time, so I am anxious to get started.
Saturday, May 29, 2010
VAC Therapy

Vacuum assisted closure has been around for a while now, and I have certainly witnessed its ability to close a gnarly wound. It really does appear to work better than the old fashioned wet-to-dry dressings. But I've wondered what really goes into the wound healing process using this system. I've learned that the negative pressure dressing applies forces inducing macrostrain and microstrain.
Macrostrain you see immediately when the suction is turned on and the wound edges are brought closer together. The suction pulls off infectious materials and edema. The pressure of the sponge against the wound bed also induces microstrain, essentially stretching of cells. The cells respond to this stain by expressing different receptors on the cell surface that ultimately promote healing. Through this there is an increase in cell proliferation, extracellular matrix production, wound perfusion, and the subsequent formation of granulation tissue.
For those that haven't worked with VAC therapy, you place foam directly on the wound bed and cover with a transparent plastic adherent. Then you have to snip a few holes in the plastic where you will attach the suction tubing. The fluids are pulled from the wound, through the sponge, and travel through the tubing into a canister. Above is a picture a VAC sponge, applied to presumably a sacral decub, with suction turned on. The little ring in the middle the black sponge is part of the tubing- this ring/circle is what you place over the holes you made. You can also see the plastic around the sponge on normal skin. When VACs are removed, you see the characteristic little bumps or ridges formed by the sponge in [hopefully] healthy tissue.
Tuesday, May 25, 2010
Spine fractures

I've found that a lot of people think paralysis occurs when they hear someone "broke their back." From my experience, though, most of the spine fractures I see do not result in paralysis. Of course, a severe fracture absolutely can result in paralysis, but I find the majority of spine fracture are not that severe.
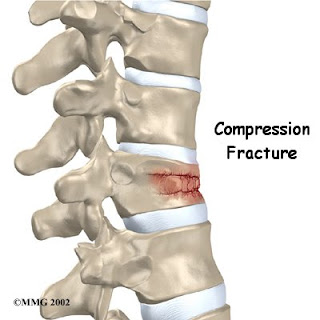
There are different types of fractures, which can involve different levels and different parts of the vertebra. Seemingly the most benign is a transverse process fracture (bony projections off the back of the vertebra, which are essentially non-weight-bearing elements). Most problems occur when the vertebral body is involved. But even with compression fractures of the vertebral body, surgery doesn't often seem required and usually treatment is a brace. Surgery would likely occur in cases involving neuro deficits, parasthesias, and/or bony fragments impinging on the spinal canal. In my previous job, in Interventional Radiology, we did a lot of vertebroplasties and kyphoplasties for compression fractures. In my current position, the Spine team almost always opts for a brace. I think I've only had 1 patient get a verteroplasty here. That is, of course, if surgical decompression isn't needed. So treatment may vary according to facility. Depending on the severity of the injury, you may get a brace, you may get a vertebroplasty/kyphoplasty, or even surgical decompression. But it may help to know if you "break" your back, it does not mean guaranteed paralysis.
Tuesday, May 18, 2010
Impact of drinking alcohol on healthcare

I just read an article that came out this month about alcohol use and it's impact on the healthcare system. I was quite surprised to learn that high-risk alcohol drinkers were less likely to access healthcare than other drinkers and that the level of risky of drinking did not predict healthcare usage.
First, I was surprised by this based on my observations in the hospital. I see a lot of people admitted as a result of heavy drinking and figure they wouldn't be in the hospital if it weren't for the fact that they had been drinking. Second, my surprise was compounded when the article started out discussing how risky alcohol use is associated with over 60 medical conditions, such as hypertension, liver disease, or coronary artery disease. And that, with 3/10 American adults engaging in risky drinking, exceeding the low-risk drinking pattern is 4x more prevalent that diabetes or 10x more prevalent than cancer. Wow. Impressive numbers, I think. And to me those impressive numbers would correlate to healthcare usage. So interesting that it doesn't!
Friday, April 23, 2010
Traumatic Pancreatitis
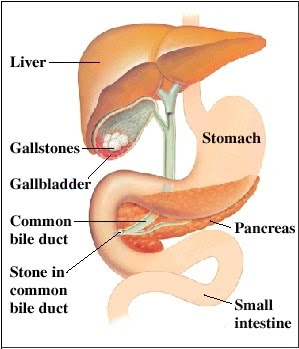
I recently had a patient that we decided had traumatic pancreatitis. The attending physician had mentioned he hadn't seen a case of this in a long time, and I'm thinking I haven't seen a case prior to this. That sort of made me think, was it more common years ago? This phenomenon isn't something I see even on occasion, or that I can think of.
Our patient had no external signs of injury and the trauma workup was essentially negative. There was some "haziness" at part of the pancreas on CT scan (can't remember if it was the head or tail), but no injury called on the read. The only thing was the patient had elevated pancreatic enzymes. In looking at some research, traumatic pancreatitis is frequently the result of trauma to the epigastrum, such as impact from a steering wheel or handle bars. If I remember, our patient was assaulted/kicked, but to the back, not abdomen.
The process is thought to involve the rupture of minor components of the pancreatic duct system, consequently releasing the enzymes. This would account for our patient's elevated levels. Management is non-operative and it will resolve naturally. From my experience, this isn't something encountered everyday, nor is it something of major concern. However, it was something new that I thought I'd share. Maybe someone else will have a case of traumatic pancreatitis soon.
Friday, April 9, 2010
Penetrating Trauma

I'm pretty sure I haven't covered this topic. I think I was about to go into impalements in my foreign objects blog, but realized it deserved it's own sections. Alas, here it is! A recent patient reminded me of this topic, as she was impaled in the eye with a pole that extended into the brain. At my trauma center, blunt trauma is far more common than penetrating trauma, so these cases are always of interest to me.
Although we do see gunshot wounds (GSW) to the head, which seem to come from Mexico with a bad story behind it, I have to say a nail gun to the head is far less frequent. But apparently it happens. In one such case, the nail hit a cerebral vessel that I don't remember anymore, but I found the case very interesting. In order to remove the nail, the patient had undergone a balloon study to determine if the patient could survive without blood flow through that vessel. The patient passed the test, so went on to have the vessel coiled, which essentially blocks blood flow permanently (which is why they had to make sure the patient could tolerate such a procedure). THEN, the nail could be removed. Quite interesting.
Speaking of GSW to the head though, sometimes they are self inflicted. A memorable example of that was a patient that shot himself in the temple, realized he was "unsuccessful" for suicide, and shot himself in the other temple. Unfortunately, this resulted in severing the optic nerve and rendering the patient blind (but the brain was completely unharmed).
In other case, a girl fell several stories onto a iron fence, impaling her vagina. I didn't see this patient, so not sure the extent of the injuries, but the mechanism was certainly enough for me to remember.

This photo avove isn't from our center, but this sort of neck trauma isn't all that rare. I've had several cases of severe neck lacerations, including injury to major vessels. Sometimes, although much less, there can be tracheal injury as well. This isn't impalement, but certainly penetrating trauma. If you get them soon enough, they actually do pretty well. It's really all about the clock-stop the bleeding in time.
Most common to our trauma center are stab wounds. I know I've seen on TV-trauma telephone poles go through torsos, but I've never had a case with that. Nonetheless, we have so many car crashes, falls, and assaults that even stab wounds are different and interesting. And anything more is just plain exotic!
Tuesday, April 6, 2010
A decision has been reached!
Well, as some of you might remember, I mentioned going back to school for a PhD. The grueling application process is over, and I recently made my official decision on which offer to accept. It was actually far more taxing than I anticipated! I only applied to 4 schools, but it turned out to be far more work than I expected when I started! I'm trying to remember if it was this much work to apply to go to school before, and I'm pretty sure it wasn't. Nonetheless, that part is over and that's a relief. Although I do realize, this is really only the tip of the iceberg! Now it's on to four years of school!
This also means a move across the country...again. I moved for school on the east coast twice, and looks like I've committed to doing the same for my PhD. It's already feeling more complicated at this age. Wish me luck in selling my house!
Regardless of the obstacles, I am excited. I look forward to the work ahead of me, even though I know it won't be easy. This will probably change my focus here, as well. When I first started this, I wanted to try make sure it wasn't only for NPs. That is hard at times, and I know I also tend to favor "trauma topics." I can't help it. But with my soon-to-be academic focus, I'm sure you will notice a change in topics again...but not until Fall!
Monday, March 22, 2010
One of those families

Most families are very nice and appropriately concerned for their loved one. But sometimes you get a family that is unhappy with everything. The second you walk in the door there are problems. "We don't like this...We don't like that...We don't know anything...We don't know why this...We want this...We need that, or else..." Sometimes there truly is a reason for all the gripes. Recently we had a patient that was transferred from another hospital, and the transferring hospital made a whole bunch of promises about what and how we were going to do things, some of which were not even possible. I was under fire the second I walked in the door. Then, as I listened more, I also realized many of the problems actually occurred at the other hospital. Wounds weren't cleaned there, there was a delay in treatment there, they were "forced" to transfer from there...and that carried over to us. "Why haven't we been seen by so-and-so? That team didn't even know about us until this morning. Why hasn't he been to surgery?" After a good hour of explanations and troubleshooting, we started to see eye-to-eye.
Fresh off that family, I got a new one. Not a transfer this time, though. They don't want these surgeons, they don't want residents, and they want everything NOW. Although I consider myself very good with patients and families, I have learned there are some cases where you can never make a family happy. You can't make enough accommodations, say enough nice things, jump through enough hoops to make them happy. Maybe some people are just predisposed to being angry everywhere they go. Maybe it's the stress of the situation that makes them think with cloudy reason. Maybe they had a prior experience that makes them go into attack-mode. I'm sure there are a whole host of explanations, but it definitely makes caring for that patient so much more difficult. Irregardless though, I still try my darnedest to make them happy, even if I never to. I can't say it doesn't make me not want to trade them in for a a nice family though.
Sunday, March 7, 2010
trauma in the elderly

I love old people. I always have, but in my nursing career I chose trauma (because obviously I love that, too). So naturally, when I started working this job in trauma, I've been interested in trends of trauma in the elderly. I started taking this interest serious enough that I looked into ways of getting more involved with the elderly and investigate data our hospital. The data I gathered is what I presented at the AANP conference last year and then submitted an article on, also. Well, it appears my interest in trauma in the elderly is catching on at my hospital. One of our fellows did a presentation on trauma in the elderly and everybody wanted me to be there. As long as I am working that day, I try to go to conference every week, so really I would have been there anyway. But it occurred to me that my interest in this topic must be well-known, or it wouldn't be that important I be there.
 Anyways, I, of course, found the presentation very interesting. One thing that I found very interesting was regarding head trauma. Now, I know I did a relatively recent blog about head bleeds, so it's going to look like I have big thing for head bleeds. I don't really have a specific interest in it; it's more because head bleeds are a common sequela of trauma. And this injury is very much seen in the elderly. There is usually a lot of discussion about elderly being on anti-coagulants (like coumadin, plavix, etc.) and its associated risk for head bleeds. But not all elderly that get a head bleed from trauma are on anti-coagulants (although, yes, it is more likely when they are taking those meds). But, it is also more common for elderly overall to get a head injury compared to their younger counterparts.
Anyways, I, of course, found the presentation very interesting. One thing that I found very interesting was regarding head trauma. Now, I know I did a relatively recent blog about head bleeds, so it's going to look like I have big thing for head bleeds. I don't really have a specific interest in it; it's more because head bleeds are a common sequela of trauma. And this injury is very much seen in the elderly. There is usually a lot of discussion about elderly being on anti-coagulants (like coumadin, plavix, etc.) and its associated risk for head bleeds. But not all elderly that get a head bleed from trauma are on anti-coagulants (although, yes, it is more likely when they are taking those meds). But, it is also more common for elderly overall to get a head injury compared to their younger counterparts.Ah, so here comes the part I find interesting. I guess I had just never connected the dots, but as we age we lose cortical brain volume. Most of us probably know that, or least knew that at one point. There is a 15-20% reduction between the 5th and 10th decade of life, such that the elderly brain only occupies 82% of the cranial vault (whereas it's 92% for younger brains). Above is a normal head CT, but with obvious volume loss. But while the brain shrinks, the dura remains adherent to the skull, increasing the subdural space and the tension on vessels (parasagital and branching veins). Studies show elderly are 3 times more at risk for a subdrual hematoma (SDH) and now it makes sense why that type specifically!
Friday, March 5, 2010
compartment syndrome
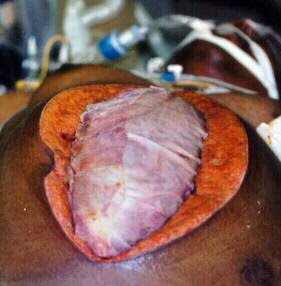
I always think abdominal compartment syndrome in an interesting phenomenon. We haven't had a case of it for a very long time, and it seems to be pretty rare from my experience, but still interesting. What made me think of it was a recent patient that thought he had compartment syndrome of his leg. Although compartment syndrome is well recognized in the extremities, this guy DID NOT have it. I'm not sure if someone told he has or may get it when he first came in, but his leg was a soft as could be. Nonetheless, he got me thinking about it and how it can also occur in the abdomen.
Compartment syndrome occurs when there is increased pressure within a fixed compartment that is usually limited by bone and/or fascia. In the abdomen, the result of this is organ dysfunction, such as decreased urine output from decreased renal perfusion or respiratory distress from decreased tidal volumes. It may seem a little strange to think of the abdomen as a fixed compartment. An extremity presents a clearer picture because its ability to distend is pretty limited. But even the abdomen will reach an endpoint in its ability to distend, as the picture above shows.
The abdomen can be at risk for compartment syndrome in an acute setting from an internal source such as intraperitoneal hemorrhage, an external factor that limits the belly from distending such as debris or structures crushing the patient, or even large volume resuscitation. An example of a chronic cause would be ascites from cirrhosis.
The key to resolving the sequela is to remove the pressure. This can be done by removing the external source or draining the internal source. Although patients with chronic ascites often undergo paracentesis (get "tapped"), this is probably not the best solution for someone who came in as a trauma patient. Most likely there is extensive internal bleeding, and merely draining the blood will not solve the problem. This would be a clear indication for going to the OR for an ex-lap to find the source of bleeding and repair it. But if there's that much blood, in some ways the pressure may be tamponading the source. In which case, once the belly opens, surgery could be quite tenuous and possibly a time when a patient "bleeds out."
Wednesday, February 24, 2010
Inmate trauma

I thought I'd cover the orange jumpsuit population since I work at the only hospital contracted to accept these patients in our county. Although it isn't the bulk of our patient population, we certainly do get incarcerated victims. Interestingly, the most common trauma mechanism in jail is blunt assault, whereas it is penetrating trauma (stab wounds) in state prison. The second most common mechanism is fall in jail and blunt assault in prison.
A common co-morbidity for both facility types is seizures. Psychiatric history is also common. Oftentimes these co-morbidities play a role in the inmate's trauma admission. For example, it is relatively common for an inmate to come in as a fall secondary to a seizure. Psychiatric illness can propagate an assault.
Sometimes we get inmates that come with a shady story about mechanism. You'll get a guy telling an elaborate story about how he fell getting out of the shower cell and yet his injuries are highly consistent with assault (like bilateral facial fractures!).
You also get often mysterious "fall from bunk" followed by an endless complaint of parasthesias. Of course everything must be taken seriously, just in case, so they get a full workup in hospital that include MRIs, neurology consults, neuro checks and observation. After days in hospital and the results are negative, as they often are, they go back to jail/prison.
But, despite their tendency to want to linger in the hospital, they are more often than not very polite and friendly! Perhaps it's because the environment is so different from their ususal day-to-day.
Sunday, February 14, 2010
cactus trauma?

Who would think, right? I'm not sure if I'd go so far as to say trauma, but apparently anything goes. So what happens if you have a traumatic encounter with a cactus? It is probably pretty unlikely that you will suffer penetrating trauma unless you find a cactus with particularly long spines. But what you may get is dermatitis. The picture of papules above is typical of dermatitis secondary to cactus pricks.
Dermatitis from a cactus generally occurs because of the mechanical irritation. There can be immunologic or infectious reactions as well, though. The cactus spines can scratch the skin causing wounds or excoriations, and the spines may break off in the skin or subcutaneous tissue causing papules or nodules.
Apparently it is the smaller spines that are more troublesome than the long scary ones. This is because the little ones can be barbed, making removal difficult. If they aren't removed, dermatitis can persist for months. A popular and successful method for removing this tricky bristles is to cover the area with sticky plaster or hot wax and then quickly removing it.
I have to say this is a new one for me. I didn't know this much about a cactus or cactus care until I had a recent clinical encounter with a cactus run-in. But now we all know a little more!
Friday, January 29, 2010
mixed results in articles

It appears to be a big month for discussing the nursing career in general nursing journals and magazines. Advance for Nurses highlighted "2010 Nursing Forecast" on their cover, Advance for Nurse Practitioners released their salary results in "Salary Survey Results: good news despite economy," and there's Lippincott's 2010 Nursing Career Directory that came out.
Kind of interesting to read them and come away with mixed reviews. The article Nursing (Job) Shortage discussed the difficulties new nursing grads are having in finding jobs because older nurses aren't retiring in this economy, seasoned nurses aren't venturing out for a position change right now, and the regular workers are picking up extra shifts.
On the flip side, the NP salary results article painted a different impression of the nursing profession. It discussed how healtcare jobs appeared strong, while overall other employment was bleak. It stated that healthcare actually added almost 600,000 positions and the overall NP salary increased yet again (up by >$8000).
Perhaps the difference is in being a new grad vs. already in a position. Perhaps the difference is between finding an RN job vs. an NP job. Maybe there's some bias in the articles. I'm not trying to compare apples and oranges. But I did feel there was a discrepancy among the articles in the overall outlook and impression of where our discipline stands in this economy right now.
From my standpoint, I don't feel largely impacted by the economy. I heard our hospital did a hiring-freeze, which has now been lifted. We did miss our annual pay raise, which I suppose does count for something. But I don't know of anyone who lost a job in our hospital or suffered a pay cut or cut in hours. I suppose even if I took the position that nursing has hit hard times, I have no doubt it will bounce back. The old are getting older, and there will be more and more of them to take care of. Nursing will be needed.
Wednesday, January 20, 2010
Head Bleeds
Yesterday we had a discussion about a case involving a significant head injury resulting in death. We ended up talking about different types of head bleeds and I thought it would be good to do a refresher.

Subdural hematoma/hemorrhage (SDH): This is when blood collects within the inner meningeal layer of the dura mater, the outer protective covering of the brain. The picture to the right is a CT scan showing a good sized left SDH, which you can see is also exerting midline shift to the right. (Of note when looking at CT scans, blood shows up white, air is black, brain matter grey, and the image is reversed- like a chest x-ray).

Subarachnoid hemorrhage (SAH): This is bleeding into the subarachnoid space, which is the area between the arachnoid membrane and the pia mater surrounding the brain (meaning the area between the brain and the thin tissues that cover the brain). The SAH image to the left shows blood in bilateral sylvian fissures and down the center interhemispheric fissure. The 2 white spots toward the back are not blood but rather normal calcifications.

Intraparenchymal hemorrhage (IPH): This is where there is bleeding into the tissue of the brain. Pretty obvious, that white blotch on the left.

Epidural hematoma (EDH): This is where blood collects between the dura mater and the skull. This is outside the dura, whereas the SDH was below the dura. It's pretty hard to miss that EDH imaged to the right, which is causing midline shift and compression of the left ventricle.
Question: How can someone status post craniectomy (bone flap NOT replaced) still have elevated ICPs?
Answer: Even with a bone flap missing, neurosurgeons almost always still close the dura, which is that tough outer membrane. The dura is tough enough to still limit significant cerebral edema and impose pressure, therefore raising ICP (intracranial pressures).

Subdural hematoma/hemorrhage (SDH): This is when blood collects within the inner meningeal layer of the dura mater, the outer protective covering of the brain. The picture to the right is a CT scan showing a good sized left SDH, which you can see is also exerting midline shift to the right. (Of note when looking at CT scans, blood shows up white, air is black, brain matter grey, and the image is reversed- like a chest x-ray).

Subarachnoid hemorrhage (SAH): This is bleeding into the subarachnoid space, which is the area between the arachnoid membrane and the pia mater surrounding the brain (meaning the area between the brain and the thin tissues that cover the brain). The SAH image to the left shows blood in bilateral sylvian fissures and down the center interhemispheric fissure. The 2 white spots toward the back are not blood but rather normal calcifications.

Intraparenchymal hemorrhage (IPH): This is where there is bleeding into the tissue of the brain. Pretty obvious, that white blotch on the left.

Epidural hematoma (EDH): This is where blood collects between the dura mater and the skull. This is outside the dura, whereas the SDH was below the dura. It's pretty hard to miss that EDH imaged to the right, which is causing midline shift and compression of the left ventricle.
Question: How can someone status post craniectomy (bone flap NOT replaced) still have elevated ICPs?
Answer: Even with a bone flap missing, neurosurgeons almost always still close the dura, which is that tough outer membrane. The dura is tough enough to still limit significant cerebral edema and impose pressure, therefore raising ICP (intracranial pressures).
Friday, January 15, 2010
Haiti Relief

As we all know, unless you're under a rock, there was a large earthquake in Haiti earlier this week that resulted in thousands of deaths and massive destruction. Well, does anyone remember my blog about the new nursing super-union? In response to this tragedy, they have issued an urgent call for nurse volunteers to help in "Earthquake Ravaged Haiti." The National Nurses United activated its nationwide disaster relief program to recruit nurse volunteers to help residents of Haiti following the earthquake devastation. Just to remind everybody, the 150,000-member NNU was formed last month through the unification of California Nurses Association/National Nurses Organizing Committee, United American Nurses, and Massachusetts Nurses Association.
“Nurses will be fundamental to the disaster relief process, to provide immediate healing and therapeutic support to the patients and families facing the devastation from this tragic earthquake,” the Co-Executive Director, Rose Ann DeMoro, said. They are working on sending nurses to provide emergency short and long term medical support, as they have done in previous major disasters, such as Katrina.
Wednesday, January 13, 2010
What else can I be?
I get asked a lot about my job. What is a nurse practitioner? What do you do? How are you different than a doctor? How are you different than a nurse? And in one of my first blogs I discussed a lot of this. But I also get asked what career alternatives are out there. So I thought I'd mention a few other career options if you think healthcare is for you but not sold on being an NP.
Probably the most similar job is a physician assistant, aka a PA. Like NPs, they diagnose, treat, manage patient's care, prescribe, and order and analyze labs and studies. The main difference is that NPs practice under the nursing model and PAs practice under the medical model, like physicians. Training is also different. NP programs entail earning an MSN (master's in nursing) degree in an area of specialty (acute care, adult, pediatric, etc). PAs spend generally 2 years studying general medical and surgical care.
If you are interested in anesthesia, you should definitely consider becoming a Certified Registered Nurse Anesthetist (CRNA). This is also an advanced practice nurse, requiring a master's degree, and that allows you to deliver anesthesia. Of the practicing CRNAs they are 51% females and 49% males. This is the nursing version of an anesthesiologist.
If you are interesting in delivering babies, you should consider being a nusre midwife. Once again, this is a master's prepared advanced practice nurse, and is similar to an OB/GYN physician. Midwives tend to care for the pregnancies in the no to low-risk category and practice under the nursing model.
There are far more options for a career in healthcare other than these mentioned, but these are options that could be considered largely on par with choosing a career as a nurse practitioner. You could also work as a registered nurse, physician, clinical nurse specialist, nurse researcher, physical or occupational therapist, respiratory therapist, and more. With so many options, you're bound to find a niche that works for you!
Probably the most similar job is a physician assistant, aka a PA. Like NPs, they diagnose, treat, manage patient's care, prescribe, and order and analyze labs and studies. The main difference is that NPs practice under the nursing model and PAs practice under the medical model, like physicians. Training is also different. NP programs entail earning an MSN (master's in nursing) degree in an area of specialty (acute care, adult, pediatric, etc). PAs spend generally 2 years studying general medical and surgical care.
If you are interested in anesthesia, you should definitely consider becoming a Certified Registered Nurse Anesthetist (CRNA). This is also an advanced practice nurse, requiring a master's degree, and that allows you to deliver anesthesia. Of the practicing CRNAs they are 51% females and 49% males. This is the nursing version of an anesthesiologist.
If you are interesting in delivering babies, you should consider being a nusre midwife. Once again, this is a master's prepared advanced practice nurse, and is similar to an OB/GYN physician. Midwives tend to care for the pregnancies in the no to low-risk category and practice under the nursing model.
There are far more options for a career in healthcare other than these mentioned, but these are options that could be considered largely on par with choosing a career as a nurse practitioner. You could also work as a registered nurse, physician, clinical nurse specialist, nurse researcher, physical or occupational therapist, respiratory therapist, and more. With so many options, you're bound to find a niche that works for you!
Saturday, January 2, 2010
Happy New Year

Happy New Year to everyone! And let me tell you, people celebrated! Wednesday before New Year's eve was not too bad in the hospital, but they certainly started rolling in on New Year's eve. In fact, they started coming in around 9am and really just kept coming for the next 24hrs. Fortunately I anticipated this and had a big push for any possible discharges that could be done the day before. That actually cut our list down to half. But on New Year's eve, a new one came in about every 30 minutes during the day and there were 20+ new admissions overnight. That's a whole bunch of new people to round on the next day. But I'm sure it could still be worse.
So let me say, I just do not understand our radiologists. I waited ALL DAY for radiology reads to come back so I could clear c-spines and dc people. I paged them multiple times, and they just couldn't get it to move faster. All I'd get is, "Well, there are a lot of traumas." I'm like, yeah, I know, I'm taking care of all of them and they want to go! It was SO painful waiting until 5PM to get final reads. What's even more rediculous is they read the newer patients first. So I can have a guy that came in a 10am on New Year's day and he gets his CT c-spine read before someone who came in at noon on New Year's eve. Make sense of that, will you? I think for a level 1 trauma center to have radiologists this slow is a crime. The head CT attending radiologist strolls in at 3 pm to do reads. Really? That just doesn't seem right to me.
Anyway, as painful as it was, we have made it through New Years. Of course we still have to make it through Sat night, which is notoriously busy, no matter the month. And sadly it probably gave all the New Year's eve drinkers a day of recovery so they can be back at it tonight.
Subscribe to:
Comments (Atom)



