Yes, I'm back. So the semester is just plugging along and I'm now over the half-way point in the semester. At some moments it has seemed agonizingly slow, and other moments I can't believe how fast it's going. I hope the latter remains true for the entire program!
So what have I learned? What pearls of wisdom can I share with you? Hum...well, truthfully I don't think you'll find them any bit interesting. So instead of content, we'll talk big picture. I do think I am starting to get the hang of the PhD-way-of-thinking. It's a slow process, granted, but I think it is starting to come together.
It's funny though, because professors will ask, "How does this tie into your own area of interest for research?" But most of the time I think they keep you so busy there's barely any time to consider how this abstract thought relates to trauma. It's actually all the quantitative work that I like the best. All this foo-foo abstract philosophy business just doesn't move me.
But the good news is I hear the first year is the worst. Actually, I've even heard it starts to get better by second semester. It sounds like the general process is you start the program with the most abstract content and then it continues to narrow down to more concrete information as you move along. Boy , I can not wait for concrete! I think acute care people in general don't live, nor want to, in some nebulous world. So, I will continue to keep you posted. Here's hoping the fog clears soon!
Monday, November 1, 2010
Friday, October 1, 2010
Pardon the time lapse again
Well, when I posted that the PhD was likely going to involve a new way of thinking, I don't even think I realized to what extent that might be. Indeed, it is different. On one hand, it is very hard to go from being a very proficient clinician to... studying theory and philosophy.
Sadly, on the other hand, I don't even think that I can say it's hard. More or less, I feel intellectually bored. Sure, they give oodles to read, and now oodles of writing is coming down the pike, but I can't really say that I feel mentally stimulated.
Instead I find myself doing other things, like this. :) I even signed up for a 7- week course through the local community. I'm getting a chance to run more than I ever could while working as a Trauma NP. My other projects are getting valuable attention.
Yet my classmates, albeit there's only 4 of us total, say how overwhelmed they feel. I sort of feel like, "Am I missing something?" Okay granted, there's plenty to do, but it honestly feels more like busy-work than bearing true value to the real world. I'm looking for meat & potatoes. Substance. Not philosophy.
Now I don't want to be too much a downer, because that's not me, so I'm just going to hold my breath and hope for the best. Let me find a silver lining- perhaps learning how I can affect large-scale change will be next semester.
Sadly, on the other hand, I don't even think that I can say it's hard. More or less, I feel intellectually bored. Sure, they give oodles to read, and now oodles of writing is coming down the pike, but I can't really say that I feel mentally stimulated.
Instead I find myself doing other things, like this. :) I even signed up for a 7- week course through the local community. I'm getting a chance to run more than I ever could while working as a Trauma NP. My other projects are getting valuable attention.
Yet my classmates, albeit there's only 4 of us total, say how overwhelmed they feel. I sort of feel like, "Am I missing something?" Okay granted, there's plenty to do, but it honestly feels more like busy-work than bearing true value to the real world. I'm looking for meat & potatoes. Substance. Not philosophy.
Now I don't want to be too much a downer, because that's not me, so I'm just going to hold my breath and hope for the best. Let me find a silver lining- perhaps learning how I can affect large-scale change will be next semester.
Thursday, August 26, 2010
A new way of thinking
Well, Orientation has begun...and the nerves are mounting. I haven't even had my official PhD intro day yet, where I'm sure I'll hear all the nitty-gritty and panic even more. But even having lunch with a 4th-year PhD student was enlightening. I am starting to realize I will have to embrace a new way of thinking. I suppose there was some mental adjustment, if I remember, when I was learning how to practice as a nurse practitioner from bedside nursing. But this change in thinking seems even more dramatic to me. To this point, all of my training and experience in nursing is in a clinical context. But now I feel I am leaving the clinician in me behind, and have to cultivate the researcher in me. As excited as I am about learning how to be a researcher, prolific publisher, and professional expert on my topic, I realize the task is daunting. Nonetheless, I hate to completely give up clinical practice 100%; it feels weird. I asked the 4th-year PhD student her opinion on working clinically at least one day a week. She did not recommend it due to the rigors of the program. She said I will be so busy and overwhelmed that I should avoid it, if possible. While I realize she is probably right, it is a bit sad. Yet, since I can see I am in for a big change, I will certainly heed any cautionary tales at this point.
Tuesday, July 27, 2010
Oops- hiatus
Oh my goodness, look how much time I let lapse! I sure didn't mean to. But I must say, a lot has happened since I last posted. Sadly, I no longer work as a trauma NP. Not that that comes as a surprise but still sad to move on. As much as I loved my job, I had to give it up to start the new chapter of my life as a PhD student. I have now relocated across the country. And let me say, that was no easy feat.
Actually, I moved a little early because I was going to study Public Health in Boston over the summer. Well, things didn't turn out as planned. Long story short, I ended up with a moving company scam that caused me to miss orientation and the start of [summer] school. I could NOT get my furniture, and I spent so much time absorbed by the scandal. Fortunately, I did get my stuff, eventually .
So now that I have finally sorted out the all the disasters from the move, I've had a chance to start looking at what's to come. Of course, I've ended up with more time now than I had expected, since my summer studies got cut out of the mix. So, with time to stop and breathe for the first time in a long time, I think I am now starting to realize I am really going back to school. It started to become real when I saw the orientation schedule and the courses I'll begin this fall. I am getting excited, although I have to admit, a bit nervous too. But I am not one to do well with much down time, so I am anxious to get started.
Actually, I moved a little early because I was going to study Public Health in Boston over the summer. Well, things didn't turn out as planned. Long story short, I ended up with a moving company scam that caused me to miss orientation and the start of [summer] school. I could NOT get my furniture, and I spent so much time absorbed by the scandal. Fortunately, I did get my stuff, eventually .
So now that I have finally sorted out the all the disasters from the move, I've had a chance to start looking at what's to come. Of course, I've ended up with more time now than I had expected, since my summer studies got cut out of the mix. So, with time to stop and breathe for the first time in a long time, I think I am now starting to realize I am really going back to school. It started to become real when I saw the orientation schedule and the courses I'll begin this fall. I am getting excited, although I have to admit, a bit nervous too. But I am not one to do well with much down time, so I am anxious to get started.
Saturday, May 29, 2010
VAC Therapy

Vacuum assisted closure has been around for a while now, and I have certainly witnessed its ability to close a gnarly wound. It really does appear to work better than the old fashioned wet-to-dry dressings. But I've wondered what really goes into the wound healing process using this system. I've learned that the negative pressure dressing applies forces inducing macrostrain and microstrain.
Macrostrain you see immediately when the suction is turned on and the wound edges are brought closer together. The suction pulls off infectious materials and edema. The pressure of the sponge against the wound bed also induces microstrain, essentially stretching of cells. The cells respond to this stain by expressing different receptors on the cell surface that ultimately promote healing. Through this there is an increase in cell proliferation, extracellular matrix production, wound perfusion, and the subsequent formation of granulation tissue.
For those that haven't worked with VAC therapy, you place foam directly on the wound bed and cover with a transparent plastic adherent. Then you have to snip a few holes in the plastic where you will attach the suction tubing. The fluids are pulled from the wound, through the sponge, and travel through the tubing into a canister. Above is a picture a VAC sponge, applied to presumably a sacral decub, with suction turned on. The little ring in the middle the black sponge is part of the tubing- this ring/circle is what you place over the holes you made. You can also see the plastic around the sponge on normal skin. When VACs are removed, you see the characteristic little bumps or ridges formed by the sponge in [hopefully] healthy tissue.
Tuesday, May 25, 2010
Spine fractures

I've found that a lot of people think paralysis occurs when they hear someone "broke their back." From my experience, though, most of the spine fractures I see do not result in paralysis. Of course, a severe fracture absolutely can result in paralysis, but I find the majority of spine fracture are not that severe.
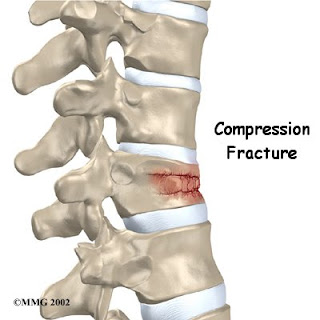
There are different types of fractures, which can involve different levels and different parts of the vertebra. Seemingly the most benign is a transverse process fracture (bony projections off the back of the vertebra, which are essentially non-weight-bearing elements). Most problems occur when the vertebral body is involved. But even with compression fractures of the vertebral body, surgery doesn't often seem required and usually treatment is a brace. Surgery would likely occur in cases involving neuro deficits, parasthesias, and/or bony fragments impinging on the spinal canal. In my previous job, in Interventional Radiology, we did a lot of vertebroplasties and kyphoplasties for compression fractures. In my current position, the Spine team almost always opts for a brace. I think I've only had 1 patient get a verteroplasty here. That is, of course, if surgical decompression isn't needed. So treatment may vary according to facility. Depending on the severity of the injury, you may get a brace, you may get a vertebroplasty/kyphoplasty, or even surgical decompression. But it may help to know if you "break" your back, it does not mean guaranteed paralysis.
Tuesday, May 18, 2010
Impact of drinking alcohol on healthcare

I just read an article that came out this month about alcohol use and it's impact on the healthcare system. I was quite surprised to learn that high-risk alcohol drinkers were less likely to access healthcare than other drinkers and that the level of risky of drinking did not predict healthcare usage.
First, I was surprised by this based on my observations in the hospital. I see a lot of people admitted as a result of heavy drinking and figure they wouldn't be in the hospital if it weren't for the fact that they had been drinking. Second, my surprise was compounded when the article started out discussing how risky alcohol use is associated with over 60 medical conditions, such as hypertension, liver disease, or coronary artery disease. And that, with 3/10 American adults engaging in risky drinking, exceeding the low-risk drinking pattern is 4x more prevalent that diabetes or 10x more prevalent than cancer. Wow. Impressive numbers, I think. And to me those impressive numbers would correlate to healthcare usage. So interesting that it doesn't!
Subscribe to:
Posts (Atom)



